Ultimovacs tar upp kampen mot melanoma
Melanom är den dödligaste formen av hudcancer och efterfrågan på nya behandlingar är därmed stor. Norska Ultimovacs är specialiserade på immunonkologi och utvecklar en typ av cancervaccin som ska stärka cancerpatienters immunförsvar. Bolagets huvudkandidat UV1 testas just nu i kliniska fas I-studier och i en fas II proof-of-concept studie där den kombineras den befintliga standardterapin för patienter med malignt melanom. BioStock fick möjlighet att prata med bolagets medicinska chef Jens Bjørheim och bolagets seniora medicinska rådgivare Steinar Aamdal för att få veta mer om sjukdomen och den pågående fas I-studie som bolaget nyligen presenterade interimresultat ifrån.
Hudcancer är en relativt vanlig sjukdom, särskilt bland individer med ljus hy vars hudceller är mer sårbara för solens skadliga ljusstrålar. Varje år diagnostiseras cirka tre miljoner människor världen över och enligt Världshälsoorganisationen (WHO) utgör hudcancer en tredjedel av alla cancerdiagnoser.
Generellt kan sägas att det finns två former av hudcancer: icke-melanom och malignt melanom. Icke-melanom hudcancer är vanligast och malignt melanom utgör bara omkring 1 procent av alla diagnostiserade hudcancerfall. Men malignt melanom är också den mest aggressiva och dödliga varianten som årligen leder till cirka 60 000 melanom-relaterade dödsfall världen över.
Därför är melanom så farligt
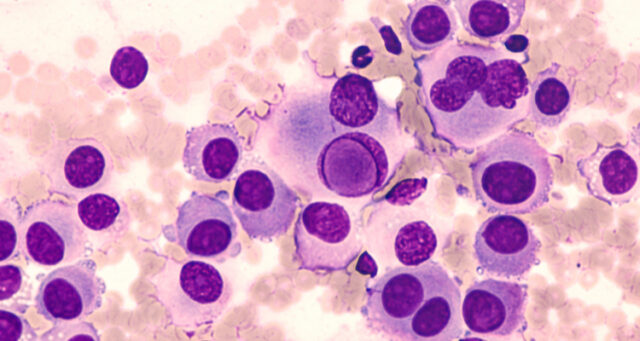
Malignt melanom bildas när DNA skadas i melanocyterna, d.v.s. hudceller som producerar melanin – det ämne som ger huden dess färg. Det skadade DNAt orsakar okontrollerad celltillväxt vilket i sin tur leder till tumörbildning. Den vanligaste orsaken till denna DNA-skada är långvarig exponering för ultraviolett strålning, som till den största delen kommer från solen. Storbritanniens National Health Service (NHS) brukar hänvisa till en studie som visar att fem eller fler solskador under barndomen kan öka risken för malignt melanom med 80 procent.
»The checkpoint inhibitors, as monotherapy or in combinations, are the most efficient current therapy for malignant melanoma and prolong patients´ survival for many years. However, since the therapy only benefits about 50 per cent of the patients, there is still a strong medical need for improving the therapeutic landscape« — Steinar Aamdal, Ultimovacs seniora medicinska rådgivare
Om malignt melanom upptäcks i ett tidigt stadium är hudtumörerna ofta relativt lättbehandlade och kan avlägsnas med ett kirurgiskt ingrepp. Men beroende på var tumören växer, stadium och genetiska profil kan även kemoterapi, strålbehandling och, på senare tid, immunterapier såsom kontrollpunktshämmare (checkpoint inhibitors) vara aktuellt.
Trots att de nyutvecklade kombinationsbehandlingarna med immunterapier kan förlänga vissa patienters överlevnad med flera år så försämras prognosen betydligt om tumören hunnit sprida sig i kroppen. Cirka en tredjedel till hälften av patienterna svarar dessutom inte på immunterapeutisk behandling, vilket då leder till dödligt utfall även med denna innovativa behandlingstyp. Med andra ord är det medicinska behovet av nya och bättre behandlingar fortfarande stort.
Ultimivacs universalvaccin genomgår kliniska studier
Ett bioteknikbolag som har identifierat detta behov är norska Ultimovacs som utvecklar en ny typ av immunterapi. Immunonkologibolaget arbetar med att ta fram ett universellt cancervaccin som kan fungera i kombination med andra former av immunterapier för att generera ett inflammatoriskt svar som skulle leda till att tumören förstörs. Läs mer om bolagets teknologi här.
 Bolagets primära kandidat är UV1, ett peptidbaserat vaccin som inducerar ett specifikt T-cellsvar mot telomeras, ett antigen som uttrycks i alla cancertyper. Ultimovacs har tidigare genomfört tre kliniska fas I-studier med UV1 där kandidaten använts antingen som monoterapi eller kombinerats med olika befintliga immunterapier i olika cancerindikationer, däribland melanom. Samtliga tre studier har konsekvent visat att UV1 är säkert och tolereras väl av patienter.
Bolagets primära kandidat är UV1, ett peptidbaserat vaccin som inducerar ett specifikt T-cellsvar mot telomeras, ett antigen som uttrycks i alla cancertyper. Ultimovacs har tidigare genomfört tre kliniska fas I-studier med UV1 där kandidaten använts antingen som monoterapi eller kombinerats med olika befintliga immunterapier i olika cancerindikationer, däribland melanom. Samtliga tre studier har konsekvent visat att UV1 är säkert och tolereras väl av patienter.
Ultimovacs har dessutom en pågående klinisk fas II proof-of-concept-studie (INITIUM) med 154 melanompatienter som utvärderar säkerheten och effekten av UV1 i en trippelkombination med två kontrollpunktshämmare, ipilimumab (Yervoy) och nivolumab (Opdivo).
Positiva resultat från fas I-studie i patienter med melanom
2018 inledde Ultimovacs en fjärde fas I-studie och den här gången testades UV1 i kombination med den vanliga kontrollpunktshämmaren pembrolizumab (Keytruda) hos 30 patienter med metastaterad malignt melanom. Den USA-baserade studien är utformad för att bedöma säkerheten och tolerabilitet för UV1 i kombination med pembrolizumab och för att undersöka initiala tecken på klinisk respons.
Patientrekryteringen slutfördes i augusti i år och bolaget rapporterade nyligen positiva resultat från en första kohort på 20 patienter. Efter att dessa patienter följts under ett år efter initial behandling kunde man konstatera att den totala överlevnadsgraden var 85 procent och att man ännu inte kunna mäta median progressionsfri överlevnad (mPFS). Det senare innebär att mer än hälften av de inkluderade patienterna ännu inte hade visat tecken på sjukdomsprogression. Det bör också nämnas att man inte fann några tecken på säkerhetsproblem relaterade till UV1 och att vaccinet tolererades väl, vilket reflekterar de positiva resultaten från tidigare fas I-studier med UV1.
Mer om melanom och den kliniska studien
BioStock kontaktade Ultimovacs seniora medicinska rådgivare Steinar Aamdal och bolagets medicinska chef Jens Bjørheim, för att få veta mer om melanom och betydelsen av de studieresultat som bolaget släppte förra veckan.
»We are very happy that the safety profile seen in the first cohort were in line with earlier studies. This tells us that it is safe to combine the UV1 vaccine with pembrolizumab. We have done an earlier study with the combination of UV1 vaccine and ipilimumab in the same indication, so now we have good safety data on combination treatment both with CTLA-4 antibody and PD-L1 antibody. This is of high importance for a good design of future combinations studies« — Jens Bjørheim, medicinska chef för Ultimovacs
Steinar, let me begin with you, could you tell us more about Melanoma and why it’s so deadly?
– Depending on the thickness of the melanoma, that is how far down into the skin the melanoma is growing, even small tumours can easily set off malignant cells into to the blood stream allowing metastases at distant sites to develop. The prognosis is serious when metastases have been established and can no longer be surgically removed.
– For many years, metastatic melanoma was an extremely difficult tumour to treat. Chemotherapy had little effect and was unable to prolong survival. It was not until immunotherapy was developed that melanoma treatment results radically changed. Immune checkpoint inhibitors became “game changers” with long-term survival benefits measured in years in many patients and in some even cures.
Why are current treatments for metastatic malignant melanoma unsatisfactory?
– The checkpoint inhibitors, as monotherapy or in combinations, are the most efficient current therapy for malignant melanoma and prolong patients´ survival for many years. However, since the therapy only benefits about 50 per cent of the patients, there is still a strong medical need for improving the therapeutic landscape.
What makes UV1 a promising candidate in your opinion, and why is it ideal for metastatic melanoma?
– UV1 is a therapeutic cancer vaccine consisting of peptides inducing CD4+ T helper type 1 (Th1) cells. These cells target the enzyme human telomerase reverse transcriptase (hTERT), which is expressed on the surface of tumour cells. That expression signals the presence of telomerase in the cell. Telomerase is an enzyme expressed almost universally in cancers and is functionally required for unlimited proliferation, which is one of the hallmarks of cancer. The selection of peptides in the UV1 vaccine is based on observation of long-time survivors (more than 10 years) in previous trials with an earlier version of the vaccine.
– UV1 may be particularly useful in melanoma since the tumour is already known to be responsive to immunotherapy. In fact, it was results from the early immune checkpoint trials in melanoma that paved the road for the general development of cancer immunotherapy. In addition, results from a previous trial with an earlier version of the vaccine in melanoma, indicated high immune responses to the vaccine.

How does UV1 differ from other classes of immunotherapy?
– The activity of checkpoint inhibitors relies on unleashing the already existing anti-tumour immune response in the patients. The UV1 vaccination, however, provides new antigens and creates new T-cells directed against the tumour, thereby broadening the anti-tumour response. In combination with checkpoint inhibitors the vaccine may enhance the anti-tumour activity of the therapy.
– Also, the UV1 vaccine can be used without pre-screening of the patients for HLA-status; it is an off-the-shelf product, easy to administer and proven to have a good safety profile in earlier trials.
– The target of the vaccine, telomerase, is present in 80-90 per cent of cancers and is therefore a potential universal cancer vaccine. A cancer expressing telomerase will do so in all cancer cells, meaning in all parts of the tumour, and will continue to do so over time, throughout the course of the cancer. This means that telomerase is likely to remain a relevant target for the immune system through different stages of a cancer and also reduces the chance of tumour escape due to heterogeneity.
Jens, turning to the clinical trial, in more details, what is the purpose of this phase I study for metastatic malignant melanoma patients where UV1 is given in combination with checkpoint inhibitor pembrolizumab?
– The primary endpoints in the trial are safety and tolerability. It is important to analyse if the combination of pembrolizumab and UV1 has an acceptable safety profile, as a guidance for further combination development.
– We have also two different cohorts in the trial: one cohort with a lower dose of the adjuvant GM-CFS (Leukine) and one with the standard, higher dose. The safety and efficacy results from the cohorts will give us valuable data in the preparation for a future filing of UV1.
Could you tell us more about the significance of the results that came out last week regarding the phase I trial?
– We are very happy that the safety profile seen in the first cohort were in line with earlier studies. This tells us that it is safe to combine the UV1 vaccine with pembrolizumab. We have done an earlier study with the combination of UV1 vaccine and ipilimumab in the same indication, so now we have good safety data on combination treatment both with CTLA-4 antibody and PD-L1 antibody. This is of high importance for a good design of future combinations studies. We have already started a phase II randomized trial in metastatic malignant melanoma where we combine the UV1 vaccine, ipilimumab and nivolumab.
– It is always difficult to interpret efficacy results from phase I studies; first, the study has a single arm design, and second, there is a limited number of patients. We observed overall survival (OS) and median Progression-Free Survival (mPFS) at one year that were on the positive side if you compare with historical controls. I think it will be very interesting to follow the data over the next years to see if the treatment matures into a superior long-term OS.
How do these results compare to previous studies conducted in metastatic melanoma patients?
– While, as mentioned earlier, it is difficult to compare with other studies, from our perspective, an appropriate historical comparison for our trial is the cohort in the KEYNOTE006 trial in which patients with advanced melanoma without prior treatment history were treated with pembrolizumab only. Results from that study demonstrated a 68 per cent OS and a mPFS of 11.6 months.
– In our trial the one-year landmark result was 85 per cent OS rate. mPFS was not reached at 12 months. We are encouraged by the results and look forward to additional data readouts over the next years that will demonstrate if the initial signs of efficacy in this cohort persist and mature into long-term added clinical benefit for the patients.

This is the second phase I trial conducted in metastatic malignant melanoma. The first trial, which was completed in 2016, was studying UV1 in combination with another checkpoint inhibitor, ipilimumab (Yervoy). What is the purpose of testing your candidate with different immunotherapies within the same indication?
– The mode of action for UV1 is to induce T-cell-recognizing telomerase (hTERT). For these cells to be effective, it is important that the treatment is combined with other interventions that allow the immune cells to attack the cancer.
– Over the last few years, we have seen that different classes of immunotherapy (CTLA-4, PD-1, PD-L1) have clinically-relevant effects in different cancer indications, e.g. malignant melanoma. The UV1 vaccine, which has a target present in 80-90 per cent of all cancers, will likely be combined with different drug combinations that improve the immune system’s ability to target the cancer in different indications. Therefore, it is also important for us to have safety and tolerability data in different UV1 combinations.
Ultimovacs also has a proof-of-concept study ongoing with 154 metastatic melanoma patients. That project is called INITIUM, and it involves a triple combination: UV1 with two checkpoint inhibitors, ipilimumab (Yervoy) and nivolumab (Opdivo). What can you tell us about this project and how does it relate with the phase I trials?
– INITIUM is a randomized phase II trial in patients with metastatic malignant melanoma. Patients that are included in the study are first-line patients, which means that they have not received cancer treatment for their metastatic disease earlier. Standard of care for a proportion of these patients is ipilimumab plus nivolumab. In our study, we randomize patients from this group to receive either nivolumab in combination with ipilimumab or nivolumab combined with both ipilimumab and UV1. Since we already have obtained safety data for UV1 combined with both PD-1 and CTLA-4 antibodies we could go directly into phase II with the triple combination.
– The INITIUM trial has already started patient inclusion, and we expect to report the primary endpoint (mPFS ) during the second half of 2022. The study will be conducted at close to 40 hospitals throughout the US and Europe.
Now that these results from the first cohort of patients (20 of 30 patients) have been published, what are the next steps for this phase I trial? When can we expect results from the rest of the patients?
– The presented results were the top-line results from the first cohort. A more detailed presentation with even more mature data from cohort 1 is planned during the first half of 2021 at an international cancer conference.
– The patients in the second cohort will have a one-year follow up in the third quarter of 2021, so next autumn both one-year data from cohort 2 and two-year data from cohort 1 will be available.
Innehållet i BioStocks nyheter och analyser är oberoende men BioStocks verksamhet är i viss mån finansierad av bolag i branschen. Detta inlägg avser ett bolag som BioStock erhållit finansiering från.



